|
BOOK NOW |
ASK ABOUT YOUR PAIN |
Home > Blog > Physiotherapy & Hand Therapy > Compartment Syndrome Physiotherapy
Compartment Syndrome Physiotherapy
Compartment syndrome is a serious medical condition that occurs when there is increased pressure in the muscular compartment of the limbs. When this pressure increases and builds up, what happens is that it causes restricted blood flow to the involved area that can compromise the health of the muscles and nerves.
Compartment syndrome is classified as either acute or chronic.
- Acute
compartment syndrome is a medical emergency, usually due to a traumatic
injury, and must be addressed immediately to avoid irreversible
consequences, such as limb loss and requiring amputations.
- Chronic compartment syndrome develops over time, usually due to excessive or inefficient exercise exertion.
Our senior physiotherapists can be effective to help identify the factors that may influence the development of compartment syndrome.
What is Compartment Syndrome?
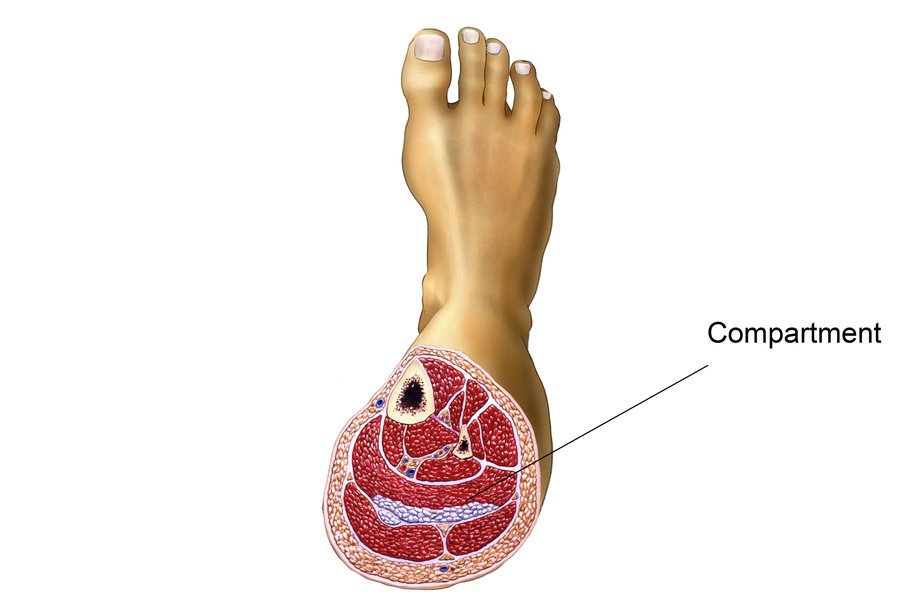
Our limbs (arms and legs) are divided into compartments that contain different muscles, nerves, and blood vessels, and each compartment is separated by fascia, which is a thick sheet-like tissue that does not stretch.
Usually, our bodies are able to handle small changes in the pressure levels within these compartments. For example, our tissues may swell slightly after a hard workout or a mild injury. But when there is excessive swelling within a compartment due to a severe acute injury or chronic overuse, pressure builds within that compartment as the fascia does/can-not expand to accommodate the increased volume.
In rare circumstances, this condition can be more than our bodies can handle, and the blood supply to the area is restricted. If the condition persists, the muscle and nerve tissue can be harmed (the pressure as well as lack of circulation can cause cells to die) - it is absolutely essential to relieve the pressure immediately to avoid permanent damage.
Acute Compartment Syndrome
Acute compartment syndrome (ACS) is a medical emergency.
It can develop as early as several hours following a severe injury and if it is left untreated for even a few hours, irreversible tissue damage can occur. ACS most often develops in the lower leg and forearm.
ACS is typically caused by a serious injury, such as:
- A direct hit or blow to the limb (athletics, a significant fall)
- Crush injuries (motor vehicle accident, work-site injury)
- Highly restrictive bandages
How Does It Feel?
The most common signs and symptoms of ACS include:
- Severe pain in the involved limb that may be out of proportion to the typical response to a certain injury
- Changes in sensation (tingling, burning, numbness)
- A sense that the limb is tight or full (from the swelling and increase in pressure)
- Discoloration of the limb
- Severe pain with stretching of the involved muscle
- Severe pain when the involved area is touched
- Significant pain or an inability to bear weight throughout the involved limb
How Is It Diagnosed?
It is critical that ACS is identified and treated immediately.
Following a severe injury, if an individual is showing signs of ACS, the individual should be taken to the emergency room right away for evaluation by a doctor. The doctor will be able to objectively measure the levels of pressure in the involved compartment. If necessary, surgery will be performed to alleviate pressure in the compartment using a procedure called a fasciotomy.
During surgery, an incision is made through the skin and fascia to drain the swelling and relieve the pressure within the compartment. A patient undergoing a fasciotomy will have to spend a period of time in the hospital to ensure that the pressure normalizes and the wound heals properly.
Following a fasciotomy surgery, physiotherapy is necessary to restore the
- motion / movement
- strength
- and function of the limb
Chronic Compartment Syndrome
Chronic compartment syndrome (CCS) is often referred to as
“exertional” compartment syndrome, and is typically caused by exercise
that involves repetitive movements, such as
- walking
- running
- biking
- jumping
Usually, excessive exercise causes the tissues of the leg to be overworked without time to recover. The development of CCS may be influenced by external factors, such as poor body control during movement, poor footwear, uneven or too-firm training surfaces, or too much training.
There have also been cases where excessive steroid use has been linked to CCS.
How Does It Feel?
The symptoms for CCS may be similar to that of ACS, but less severe and not a result of an acute traumatic injury. These may include:
- Pain and cramping in the involved limb that usually worsens with activity and subsides with rest
- Mild swelling
- Pain with stretching
- Numbness or tingling in the limb
- Weakness
How Is It Diagnosed?
Because the symptoms of CCS are similar to many other conditions, it is important that a doctor or senior physiotherapist rules out other possible diagnoses, such as
- tendinitis
- stress fractures
- shin splints
- or other inflammatory conditions
The examination may include the use of diagnostic imaging, such as an
- ultrasound
- x-ray
- MRI
to assess the tissues in the painful area.
If CCS is suspected, the patient will likely be referred to a doctor for a specific test called the "compartment pressure measurement."
This test is only used in cases where CCS is strongly suspected. It is performed in a medical office. During the test, the pressure in the involved compartment is measured before, during, and after exercise.
The goal of the test is to reproduce symptoms as they occur during real-life activities.
If CCS is diagnosed, your medical team will devise a plan to best treat your specific condition. For more mild cases of CCS, you will likely be referred directly to see our senior physiotherapists. In more severe cases, individuals are likely to be referred to a surgeon to discuss the option of a fasciotomy.
How Can our senior PhysioTherapist Help?

If you are diagnosed with compartment syndrome, our senior physiotherapist will play an important role in the treatment of the condition, whether it requires surgery or not.
We will work with you to design an individualized treatment program based on your condition and your personal goals.
Our senior physiotherapist may do these for you:
Range-of-Motion Exercises.
Restrictions in the motion of your knee, foot, or ankle may be causing increased strain in the muscles housed within the compartments of your lower leg.
Stretching techniques can be used to help restore motion in these joints to minimize undue muscle tension.
Muscle Strengthening.
Hip and core weakness can influence how your lower body moves, and can cause imbalanced forces through the lower-leg muscle groups that may contribute to compartment syndrome.
Building core strength (in the muscles of the abdomen, low back, and pelvis) is important; a strong midsection allows greater stability through the body as the arms and legs perform different motions.
For athletes engaged in endurance sports, it is important to have a strong core to stabilize the hip and knee joints during repetitive leg motions.
We will be able to determine which muscles are weak, and provide specific exercises to target these areas.
Manual Therapy.
All our senior physiotherapists are trained and experienced in manual (hands-on) therapy, using their hands to move and manipulate muscles and joints to improve motion and strength.
These techniques can target areas that are difficult to treat on your own.
Modalities.
We may use modalities e.g.
as a part of your compartment syndrome physiotherapy program. These tools can help improve tissue mobility and flexibility, and enhance recovery. We will discuss the purpose of each modality with you.
Education.
Your treatment will include education about how to safely return to your previous activities, particularly if your condition required a fasciotomy. We may recommend:
- Wearing more appropriate footwear
- Choosing more appropriate surfaces and terrain for exercise
- Pacing your activities
- Avoiding certain activities altogether
- Mastering strategies for recovery and maintenance of good health (e.g., allowing your muscles and joints proper rest time)
- Modifying your workplace to lower risk of injury