|
BOOK NOW |
ASK ABOUT YOUR PAIN |
Home > Blog > Physiotherapy > Osteoarthritis Physiotherapy > Conditions > Joint Pain > Osteochondritis Dissecans Physiotherapy
Osteochondritis Dissecans Physiotherapy

Osteochondritis dissecans (OCD) refers to a painful joint condition that involves damage to the cartilage and underlying bone within a joint. When this damage occurs, what happens is that a fragment of the cartilage comes loose from the bone.
OCD most commonly occurs in individuals between the ages of 10 and 20, typically affecting males more than females. The most common joints in which this condition occurs are the knee and the ankle, as they are weight-bearing joints.
OCD may be caused by repetitive trauma or from a single traumatic episode. If we manage to identify it early, OCD is a condition that can be effectively treated by our senior physiotherapists.
What is Osteochondritis Dissecans?
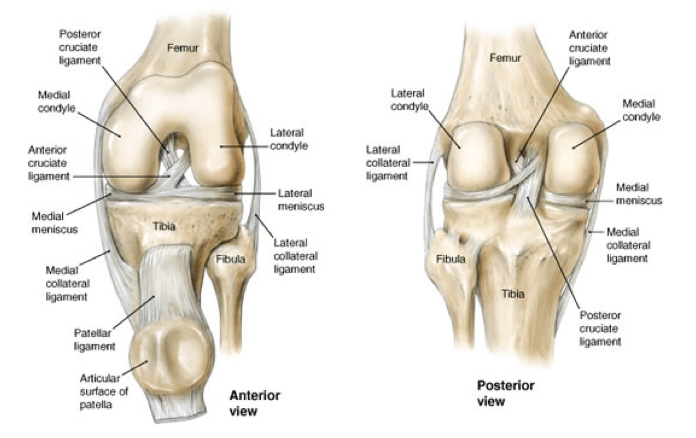
Osteochondritis dissecans (OCD) happens when there is injury to cartilage within a joint. Cartilage is a tissue that lines the ends of bones; its primary purpose is to provide a smooth surface that decreases the friction where bones meet to form joints. Our cartilage also helps to lessen the forces that go through joints.
The process leading to OCD begins when the blood supply to the layer of bone that lies directly under the cartilage layer drops. As a result of this, the bone does not receive the nutrients from blood that it needs to maintain its normal structure, and begins to die.
This process is called avascular necrosis.
When the health of the bone decreases, the cartilage does not have a good support system, and becomes susceptible to injury. If there is continued load applied to the joint (eg, repetitive walking, running, jumping, landing), a cartilage fragment may break off and then dislodge from the bone.
When this occurs, it can lead to a cascade of symptoms, including
- pain
- inflammation
- and decreased function
How Does Osteochondritis Dissecans Feel?
Common signs and symptoms that develop with OCD include:
- Swelling of the affected area following activity
- Restricted joint movement (range of motion)
- Pain when moving the joint
- Tenderness to touch along the affected joint
- A feeling of "popping," cracking, or grinding when moving the affected joint (this sound is known as "crepitus"); joint pain, joint stiffness, or "locking" (such as locked knees) after sitting with the knee bent or straight for a prolonged period of time
- Worsening pain during or following activity, particularly with walking, running, jumping, or changing direction. Children may complain of pain during physical activities, recess or gym activities.
Typically, symptoms of Osteochondritis Dissecans develop gradually as the damage to the cartilage and bone progresses.
In fact, sometimes, individuals do not recognize that they have OCD because
- they cannot remember a specific time or injury that caused their pain
- or their initial symptoms are not enough to completely restrict their activity
This is especially common with children, who may not recognize that anything is wrong or be able to describe their symptoms. However, if untreated, the degree of OCD can progress and make treatment more difficult.
How Is Osteochondritis Dissecans Diagnosed?
The first step to diagnosing OCD is to have a thorough clinical examination.
Our senior physiotherapists will ask about your medical history and activity regimen. We will perform a physical exam to measure the affected joint's
- movement (range of motion)
- strength
- mobility
- flexibility
You might also be asked to gently perform movements to provoke the pain you are experiencing.
Younger children may require the help of a parent or guardian to detail their complaints and behavior changes in response to symptom development. The child’s teacher or athletic coach may also be able to provide information specific to how the child responds to certain physical activities during the school day.
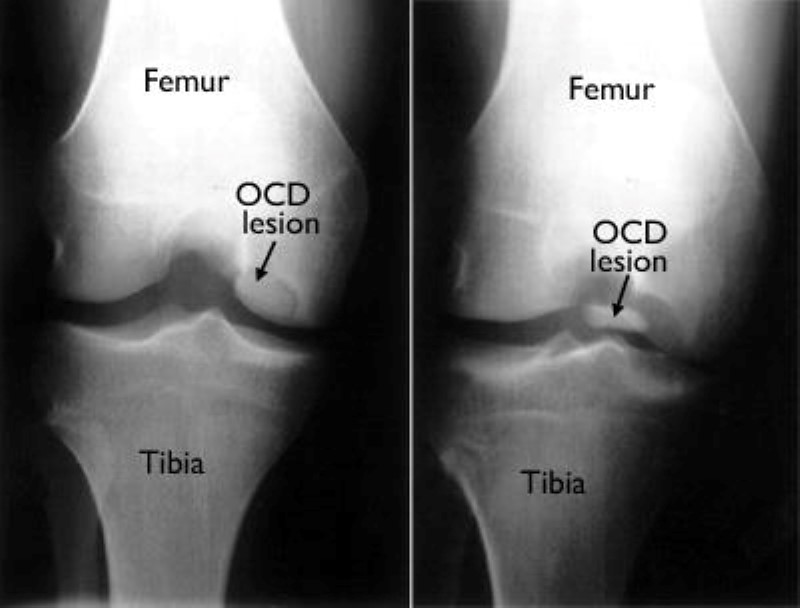
The second step in the diagnosis process is the use of medical diagnostic imaging.
We may refer you to a physician, who will order x-rays of your joint in a variety of positions to assess weight-bearing effects on it (eg, walking, standing). If more severe joint damage is suspected, an MRI or CT scan may be ordered to look more closely at the overall status of the joint and surrounding tissues.
Your medical team will grade the status of the affected bone and
cartilage based on your MRI findings, and assign it a point on a scale.
If surgery is required, an additional scale will be used to label the
level of damage present. These scales will be helpful as we develop an individualized rehabilitation program.
OCD may also occur in conjunction with other joint injuries. Therefore, it is important that the medical team use thorough diagnostic tests to ensure all injuries are identified as treatment plans are developed.
If you have joint pain that is not responding to rest (or seem to be getting worse), please seek
the advice of a medical provider!
how our senior physiotherapists can help

We will design an individualized treatment program specific to the nature of your condition and your goals.
Your physiotherapy treatments may include:
Range of Motion Exercises
One of the most common symptoms of OCD is abnormal motion of the affected joint. We will assess your motion compared to expected normal motion, and the motion of the uninvolved joint on the other side of your body.
Muscle Strengthening
Strengthening the muscles around the injured joint is an essential part of the rehabilitation program. When there is an injury to a joint that causes pain and swelling, muscles often become inhibited, which means they may not function at their normal capacity.
In the event of OCD, decreases in muscle performance may not be obvious at first, but may worsen as the degree of damage to the cartilage and bone progresses. For example, as the muscles along the front and back of the thigh (the quadriceps and hamstrings) cross the knee joint, they help control the motion and forces that are applied to the bones of the knee.
Strengthening the hip and core muscles can also help balance the amount of force on the joints of the leg, particularly during walking or running. We will assess these different muscle groups, compare the strength in each limb, and prescribe specific exercises to target your areas of weakness.
Manual Therapy
We're trained in manual (hands-on) therapy.
We will gently move and manipulate your muscles and joints to improve their
- motion
- flexibility
- strength
These techniques can target areas that are difficult to treat on your own. In patients with OCD injuries, manual therapy techniques can help to restore the joint's normal motion.

Modalities
We may recommend therapeutic modalities, such as
- cold therapy
- heat therapy
- ultrasound therapy
- radio-frequency Indiba physiotherapy
- deep tissue release
- manual therapy
- dry needling
- joint mobilization
- stretching exercises
- strengthening exercises
to aid in pain relief physiotherapy management.
Bracing
Compressive sleeves placed around the affected joint may help reduce pain and reduce swelling.
In the event that surgery is required, braces may be used to control the amount of motion that is allowed as the postsurgical rehabilitation program progresses.
For example, if an OCD injury at the knee joint is treated surgically, a brace will keep the knee straight for the first several weeks after surgery.
Activity Guidance
Since OCD may progress slowly over time, our senior physical therapist will use your symptoms as a guide to prescribe activity levels that will help and not harm your joint. We will consider the stage and extent of your OCD, and recommend a specific exercise program to address your needs and maximize the health of the affected joint.
Consultation with your physician regarding periodic diagnostic imaging will help make sure that the cartilage and bone are ready to withstand certain loads.
Surgery Considerations.
When conservative management strategies are not successful in the treatment of osteochondritis dissecans, or in cases where there are other associated injuries, surgery may be considered. The goal of surgical intervention is to restore the area of damaged cartilage and bone.
There are many factors to consider when determining the appropriate surgical treatment, including the nature of your condition, your age, and your desired activity level. We will refer you to an orthopedic surgeon to discuss your surgical options.