|
BOOK NOW |
ASK ABOUT YOUR PAIN |
Home > Blog > Physiotherapy > Conditions > Heel Pain > Plantar Fasciitis Physiotherapy
Plantar Fasciitis Physiotherapy
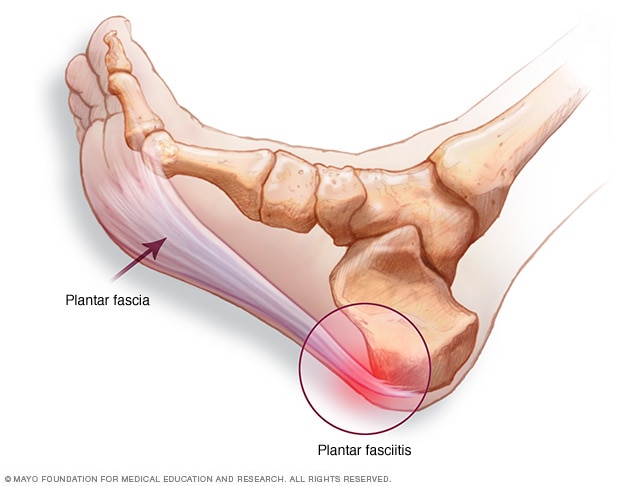
Plantar fasciitis refers to a painful heel and plantar fascia condition causing heel pain.
What happens is that the plantar fascia, which is a thick band of tissue connecting the heel to the ball of the foot and supports the arch, can become
- inflamed
- micro-tears
It results in patients experiencing pain when they step or put weight on their affected foot—particularly when taking the first steps in the morning. The pain can be felt at the heel, or along the arch and the ball of the foot.
Actually, plantar fasciitis is a common foot condition.
It happens in as many as 2 million Americans per year and 10% of the population over their lifetimes...and our senior physiotherapists do treat a lot of plantar fasciitis conditions in our physio clinics.
Factors that contribute to the development of plantar fasciitis include:
- Age (over 40 years)
- A job, sport, or hobby that involves prolonged standing or other weight-bearing activity
- Rapid increases in length or levels of activity, such as beginning a new running program or changing to a job that requires a lot more standing or walking than you are accustomed to
- Decreased calf muscle flexibility
- Increased body weight (Body Mass Index greater than 30) (being overweight and obesity plays a part)
- Tendency to have a flat foot (pronation)
Plantar fasciitis affects people of all ages, both athletes and non-athletes. Men and women have an equal chance (50-50%) of developing the condition.
Plantar fasciitis physiotherapy treatment generally
- reduces pain and
- restores your ability to put weight on your foot again
What is Plantar Fasciitis?
Plantar fasciitis is a condition causing heel pain.
Supporting the arch, the plantar fascia, a thick band of tissue connecting the heel to the ball of the foot, can become inflamed or can tear. The condition develops when repeated weight-bearing activities put a strain on the plantar fascia.
Patients who are diagnosed with plantar fasciitis also may have heel spurs, which refers to bony growth that forms on the heel bone. However, unlike PF, patients with heel spurs may not experience pain.
Plantar fasciitis occurs most frequently in people in their 40s but can occur in all age groups.
The condition can develop in athletes who run a great deal and in non-athletes who are on their feet most of the day, such as
- police officers
- cashiers
- restaurant workers
- healthcare professionals such as doctors, physiotherapists (yes us too! As we tend to be on our feet the entire day)
- etc
Signs and Symptoms
The onset of symptoms of plantar fasciitis typically and frequently occurs with a sudden increase in activity frequency and intensity.
You might feel a stabbing pain on the underside of your heel, and a sensation of tightness and/or tenderness along your arch.
People with plantar fasciitis may experience pain:
- In the morning, when stepping out of bed and taking the first steps of the day
- With prolonged standing
- When standing up after sitting for awhile
- After an intense weight-bearing activity such as running
- When climbing stairs
- When walking barefoot or in shoes with poor support
As your body warms up, your pain may actually decrease during the day but then worsen again toward the end of the day because of fatigue and extended walking.
Severe symptoms may even cause you to limp.
How Is It Diagnosed?
Our senior physiotherapists will diagnose your plantar fasciitis based on your health and activity history and a clinical evaluation.
We also will take a medical history to make sure that you do not have other possible conditions that may be causing the pain (such as heel spurs or ankle sprains or pulled calf muscles etc).
Sharing information about the relationship of your symptoms to your work and recreation, and reporting any lifestyle changes, will help us diagnose your condition and tailor a treatment program for your specific needs.
To diagnose plantar fasciitis, our senior physiotherapists may conduct the following physical tests to see if symptoms occur:
- Massaging and pressing on the heel area (palpation)
- Gently stretching the ankle to bend the top of the foot toward the leg (this movement is called dorsiflexion)
- Gently pressing the toes toward the ankle
how our senior physiotherapists can help

Physical therapists are trained to evaluate and treat plantar fasciitis.
When you are diagnosed with plantar fasciitis, we will work with you to develop a program to decrease your symptoms that may include:
- Stretching exercises to improve the flexibility of your ankle and the plantar fascia
- Use of a night splint to maintain correct ankle and toe positions
- Selection of supportive footwear and/or shoe inserts that minimize foot pronation and reduce stress to the plantar fascia
- Application of cold therapy to decrease pain and inflammation
- Ultrasound therapy and radio-frequency Indiba physiotherapy to accelerate soft tissue healing
- Iontophoresis (a gentle way to deliver medication through the skin)
- Taping of the foot to provide short-term relief
Research shows that most cases of plantar fasciitis improve over time with these conservative treatments, and surgery is rarely required.
